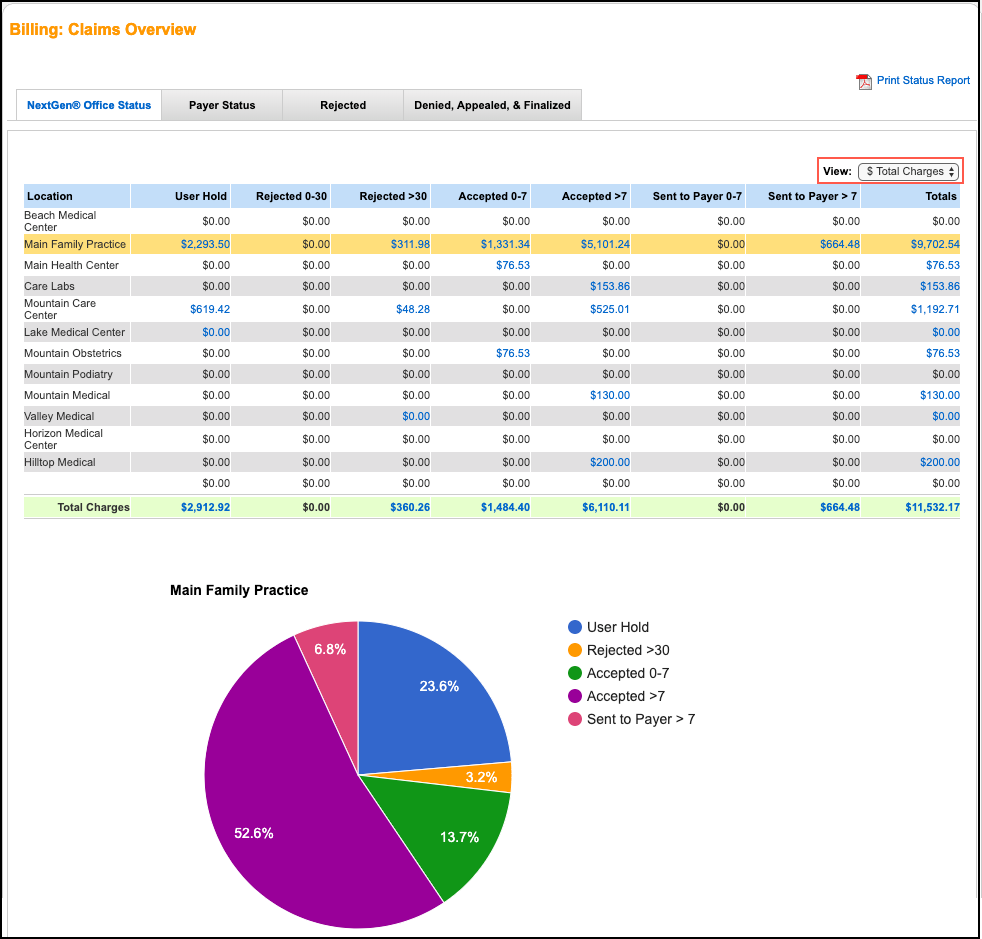
NextGen Office Claims Status Dashboard
INSTRUCTIONS:
The Claim Status Dashboard shows claims in the Electronic Data Interchange (EDI) process with a created date in the last six months. The dashboard is broken down by location and a pie chart is available for each status.
Note: We receive and process 999 acknowledgements and 277 claim status responses for all payers.
Navigate to Claim Status Dashboard
On the menu bar, click Billing, hover over Claims, and then select Claim Status Dashboard.
Claim Statuses
- To show the list of claims, click the dollar amount hyperlink.
- Use the View filter to show the $ Total Charges, the Claim Volume, or both.
NextGen Office Status
| Status | Definition |
|---|---|
| User Hold | An incomplete claim that has not yet been transmitted to the payer. |
| Rejected | Claims rejected by NextGen® Office (HF Rejected). |
| Accepted | Electronic: Electronic claims that are ready to be transmitted to the payer in the next batch (HF Accepted). Claims are batched at the end of the business day (PT). Paper: Paper claims that you must print on a CMS-1500 form (Paper Accepted). |
| Sent to Payer | Electronic: Claim electronically sent to payer and a 997 report (confirmation of batch delivery) or 999 acknowledgement was received. Paper: Paper claims that were printed on a CMS-1500 form and sent to the payer. After printing, you can mark that the print was successful. |
Payer Status
| Status | Definition |
|---|---|
| Acknowledged | Claims that were acknowledged (Received) through a claim status report (277). These reports may come from the EDI gateway or directly from the payer. A claim in the Acknowledged status does not guarantee the payer will adjudicate the claim. |
| Rejected | Claims rejected in the EDI process by the payer or the EDI gateway. |
Rejected
To edit and resubmit the claim, click the dollar amount hyperlink.
| Status | Definition |
|---|---|
| HealthFusion Rejected | Claims rejected by NextGen Office. |
| Payer Rejected | Claims rejected by the payer or the EDI gateway during the EDI process. |
Denied, Appealed, & Finalized
| Status | Definition |
|---|---|
| Received | 277 claim status report received acknowledging that an individual electronic claim has been acknowledged by the payer or another vendor. Note: If payer has not received claims, check the EOB/ERA or contact the payer for additional information. |
| Appeal | Adjudicated claims marked for appeal. |
| Denied | Adjudicated claims that were denied. |
| Finalized | If a claim is not denied and has a $0 insurance balance, the status is Finalized. Electronic: Insurance payment has successfully posted to all service lines. If no insurance payment is present, the payer may send a finalized message in the 277 claim status report. Paper: Insurance payment has successfully posted to all service lines or awaiting insurance payment posting. |
Print Status Report
To generate a PDF of the data within each tab, click Print Status Report.
Call MPM today to schedule a Demo at 973-256-1998 x2


