NextGen Office Monthly Financial Summary
Analysis Grid
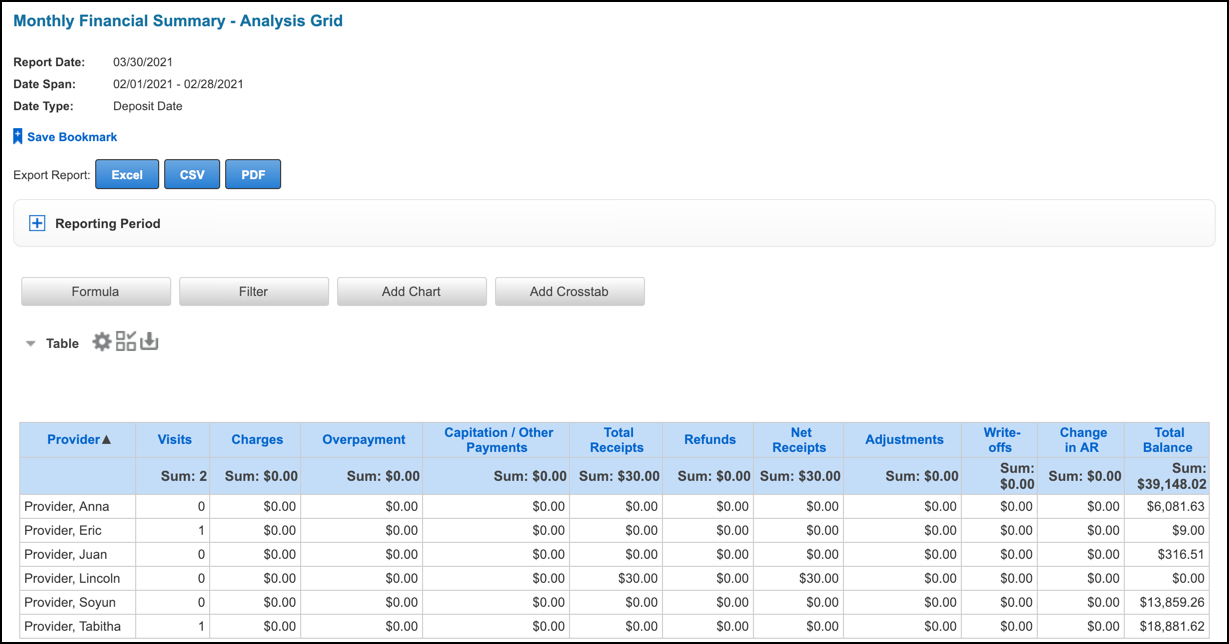
This article describes the Monthly Financial Summary Analysis Grid, which you can use to review important financial values by provider, such as transactions and payments, using a custom date span.
Highlights
- The logic used to compile reporting values is designed to match only the payment-related columns of our old Monthly Financial Summary. All other columns are calculated differently.
- We updated charges, adjustments, and write-offs to only report by the transaction’s ledger date, thus helping users comply with accurate balancing procedures. These values will not match to the old Monthly Financial Summary.
- Reporting these values by ledger date guarantees these values will not change when comparing them at two different points in time as long as the the month has been closed.
- When entering transactions, the ledger date always defaults to the current date and is thus comparable to the created date unless it is changed at the time of entry.
Recommendations
- After the month is closed, you must not void any payments posted in the system. Failure to do so will result in changes to the reported payment values for past closed months. Only ledger date-based reports will not change if payments are voided after month close.
- We recommend that you apply all payments to a claim or tag the payment to a provider before closing the month. This is necessary to confirm all payments are reported to a provider at month close. Failure to do so will result in inaccurate allocation of payments to each provider.
Reporting Data
- Combines transaction, payment, and charge data
- Data is updated daily at 11:59 PM PT
- Data is available starting January 1, 2016
Navigate to Reports
From the Practice Management menu bar, hover the cursor over Reports and then click Reports.
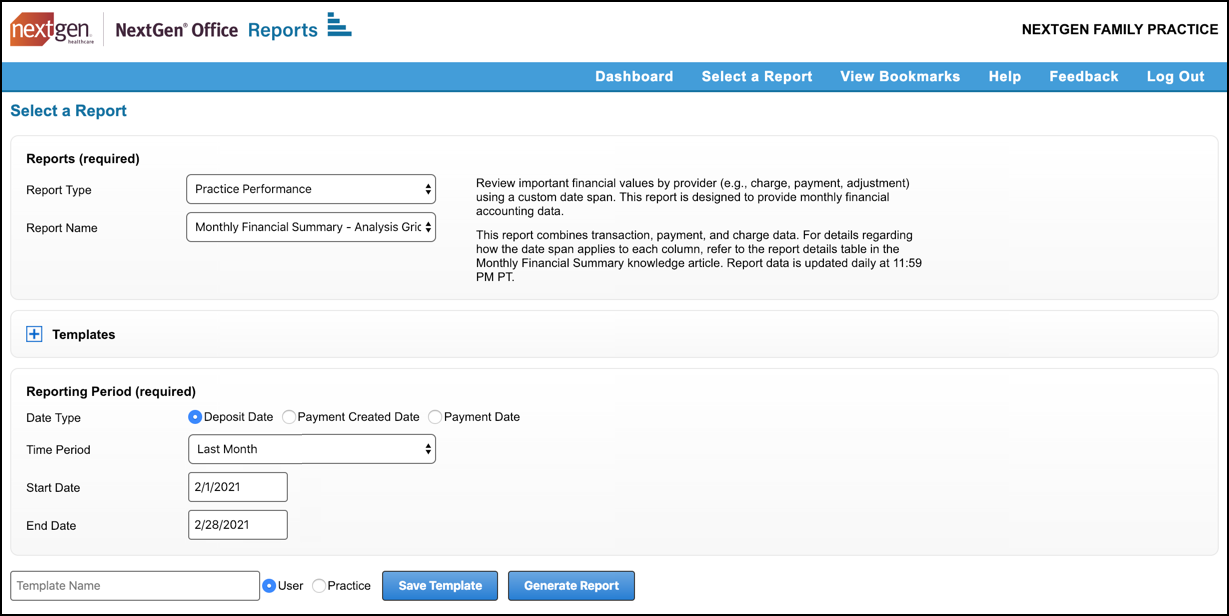
Generate a NextGen Office Monthly Financial Summary Report
- For Report Type, select Practice Performance.
- For Report Name, select Monthly Financial Summary – Analysis Grid.
- Select a reporting period.
For details on each Date Type as they relate to each report column, see Report Details.
- Select a Time Period or enter a Start Date and End Date.
- Click Generate Report.
Report Details
We define columns and date types as they related to each column. To match these columns to a detailed report, use the recommended reports in the Matching Reports column.
| Column | Definition | Deposit Date | Payment Created Date | Payment Date | Matching Report |
|---|---|---|---|---|---|
| Provider | Provider = servicing provider If no servicing provider, it is the rendering provider. If no servicing or rendering provider, it is the billing provider. |
||||
| Visits | Unique date of service per service line per patient | Created date of the service lines | Created date of the service lines | Created date of the service lines | Use the Service Line Details – Analysis Grid to calculate |
| Charges | Identifies all charge transactions that increase or decrease the insurance or patient balance. | Ledger date of the transaction | Ledger date of the transaction | Ledger date of the transaction |
|
| Work RVU |
|
Created date of the charge | Created date of the charge | Created date of the charge |
|
| Gross Applied Payments |
|
Deposit date of the payment | Created date of the payment | Payment date of the payment | Detailed Applied Payment – Analysis Grid |
| Applied Insurance |
|
Deposit date of the payment | Created date of the payment | Payment date of the payment | Detailed Applied Payment – Analysis Grid Sum insurance payments and group by servicing provider. |
| Applied Patient |
|
Deposit date of the payment | Created date of the payment | Payment date of the payment |
|
| Overpayment |
|
Deposit date of the payment | Created date of the payment | Payment date of the payment |
|
| Unapplied Payments |
|
Deposit date of the payment | Created date of the payment | Payment date of the payment |
|
| Capitation/Other Payments |
|
Deposit date of the payment | Created date of the payment | Payment date of the payment |
|
| PMT ADJ |
|
Deposit date of the payment | Created date of the payment | Payment date of the payment |
|
| Total Receipts | Formula: Gross Applied Payments + Unapplied Payments + Capitation/Other Payments + Payment Level Adjustments (PMT ADJ) | Deposit date of the payment | Created date of the payment | Payment date of the payment |
|
| Refunds | Identifies all refunds posted. | Deposit date of the payment | Created date of the payment | Payment date of the payment |
|
| Net Receipts | Formula: Total Receipts – Refunds | Deposit date of the payment | Created date of the payment | Payment date of the payment | Use formula |
| Voided |
|
Deposit date of the original payment | Created date of the payment | Payment date of the payment |
|
| Adjustments | Identifies insurance adjustment transactions by ledger date. | Ledger date of the transaction | Ledger date of the transaction | Ledger date of the transaction |
|
| Write-offs | Write-offs are reported by the ledger date. | Ledger date of the transaction | Ledger date of the transaction | Ledger date of the transaction |
|
| Change in AR | Formula: Charges – (Applied Insurance Payments + Applied Patient Payments + Adjustments + Write-offs) These are the only columns included because they are the only ones that either increase or decrease the total balance (AR). |
Use formula | Use formula | Use formula | Use formula |
| Total Balance |
|
Date of service of the charge | Date of service of the charge | Date of service of the charge | AR by Servicing Provider – Summary from the start of time until the last day of the month being closed. |
Click below to schedule a NextGen Office Demo



